Breast Cancer Risk Calculator
"Why should I assess my risk of developing breast cancer? It will not happen to me." If this has ever been you, stop for a moment and think. Breast cancer affects "1 in 8 women". Imagine eight women that you know. One of them will be diagnosed with breast cancer during her lifetime.
Even more important is this: In cases of early diagnosis, 99% of women are still alive in 5 years.
Like every year, this October is Breast Cancer Awareness Month. Health organizations around the world aim to increase the awareness of breast cancer. They aim to make the topics of prevention, diagnosis, and treatment the talk of the town. We hope to help, with our goal being to spread information on prevention and raise social awareness of early detection and diagnosis in individual women.
With this calculator, you can assess whether you're at an increased risk of breast cancer, and such should focus on prevention and screening. How? You'll find out in the article below 👇.
Risk factors of breast cancer
Breast cancer is a type of cancer that develops in the tissue of the breast.
There are some scientifically proven risk factors of developing this disease, out of which the most important ones are:
- Obesity (check the BMI calculator), and lack of regular physical activity.
- Drinking alcohol.
- Hormone replacement therapy during menopause.
- Radiation therapy to the chest.
- Beginning menstruation at an early age.
- Having children late or not at all.
- Family history of breast cancer.
Some patients suffer from so-called inherited breast cancer - this is caused by a mutation in the BRCA1, BRCA2 or other genes. A mutation in one of these genes greatly increases the risk of developing breast cancer. Therefore, it is essential to test for such mutations, especially if you have a family history of breast cancer. The test is very simple and safe for the patient - it only requires a donation of blood or saliva for examination.
The risk of developing breast cancer also increases when you suffer from atypical ductal hyperplasia. This is a benign lesion of the breast, often diagnosed after a biopsy. In spite of its benign character, it may transform into cancer, thus special treatment and management is required.
When can I use this calculator?
The answer is - practically anytime, anywhere you want (it's quick!).
However, there are some scenarios in which the tool will suggest you to consult more accurate sources. These are:
-
Previous suffering from any breast cancer, be it lobular carcinoma in situ (LCIS) or ductal carcinoma in situ (DCIS). Also, if you have received radiation therapy to the chest for treatment of Hodgkin's lymphoma.
-
A mutation in the BRCA1 or BRCA2 genes, or a particular genetic syndrome (such as Li-Fraumeni syndrome). All of the above significantly increase the risk of breast cancer.
-
Being less than 35 or more than 79 years old.
If you meet either of the first two conditions, you should consult a physician.
How does the calculator work?
The formulas applied in the breast cancer risk calculator are based on the , a statistical algorithm developed in 1989 by Dr. Mitchell Gail and his colleagues. Recently, it was adjusted for , and . Currently, it is used to assess a woman's 5-year and long-term risk of developing breast cancer.
As mentioned above, the formulas are not applicable for women with a previous diagnosis of breast cancer, a known mutation that increases the risk of developing breast cancer, or women not aged between 35-79. In the first case, a breast cancer recurrence risk calculator may be of use.
Your relative risk is a multiplication of all of the risk factors included in this model:
- Your age (AGE).
- Ethnicity (ETHN).
- Age at menarche (AGEMEN).
- Age at which you first gave live birth (AGEFLB).
- How many previous breast biopsies you have had, if any (NBIOPS).
- In the case you've had a biopsy, if the lesion was atypical hyperplasia (AHYP).
- The number of first-degree relatives diagnosed with breast cancer (NUMREL).
RR = AGE * ETHN * AGEMEN * AGEFLM * NBIOPS * AHYP * NUMREL
The values of each factor differ depending on your ethnicity and age. The model of RR and absolute risk were developed from case-control data derived from women participating in the research.
Here is a point-by-point guide on how to use this breast cancer risk calculator:
-
Input whether you have ever been diagnosed with breast cancer or have any breast cancer-associated mutations. The breast cancer risk calculator might not work correctly if you answered yes.
-
Set your race and current age.
-
Fill in the part about your medical history. In this section, you're also asked if any of your closest female relatives (mother, sisters, daughters) have been diagnosed with breast cancer.
-
Your personalized results will show your 5-year and long-term risks of developing breast cancer. You'll also find a graph showing how you compare with the U.S. population.
How to interpret the results?
There are two listed results:
-
The first numbers given is your individual 5-year risk of developing breast cancer. Just below it you can find the 5-year risk for women in the of the same age and race/ethnicity. You can also take a look at the left-hand side chart to see if your risk is higher or lower than the average. If your risk is higher than average, your results are displayed in red and orange. Otherwise, they will be blue.
-
The second set of results is your individual long-term risk of developing breast cancer. The interval here depends on your age:
- For women younger than 60 years old, it's equal to
30 years. - If you're aged 60-70, the interval is
20 years. - If you're older than 70 - the interval is
10 years.
Below you can see risk (over the same interval) for women in the general U.S. population of the same age and race/ethnicity. On the right-hand side of the chart, you can see if your risk is higher or lower than the average. If it is higher, then your results are displayed in red and orange. Otherwise, they remain blue.
- For women younger than 60 years old, it's equal to
Some research recommends that women older than 35 with a 5-year risk of 1.7% or higher (1.7% is the average risk of a 60-year-old woman) should use chemoprevention. However, it's not been decided yet what the final cutoff point should be.
👉 Long story short - if your 5-year or long-term risk is higher than average, you might need a different approach than the one mentioned in the Screening and prevention guidelines section below. Consider making an appointment with your GP with whom you can discuss your further options for screening and prevention.👈
The calculator in practice - an example
Let's take Lucy, an African-American woman, aged 54, as an example. Her mom had breast cancer, but she doesn't know if she has any of the mutations in the BRCA1 or BRCA2 genes. She had her first menstruation at the age of 12, and has two kids. She gave birth to the oldest when she was 27. She has had one biopsy so far (she had a suspicious lump), but no atypical hyperplasia was found.
Her relative risk (described above) is:
RR = 1.31 (menstruation age)* 1.07 (number of biopsies) * 1.61 (age at first birth * number of affected first-degree relatives)
RR = 2.25
The statistically-induced absolute 5-year risk for Lucy is 2%. For an average US citizen of the same race/ethnicity and age, it is 1.3%. Therefore, Lucy is at higher risk than average of developing breast cancer in the next five years.
Her projected 30-year risk is 10.5%. Again, the average US woman of the same race/ethnicity and age has an absolute risk equal to 8.4%. Lucy should consult a doctor to have her screenings more often, or have it done with more invasive methods.
What can I do?
Breast cancer is usually detected by someone accidentally discovering a lump in their breast - such as when taking a bath or getting dressed. You should know how your breasts look normally and consult a physician whenever you notice any changes.
It is recommended that you perform a at least every month during the first half of your menstrual cycle. In the second half of the cycle, just before menstruation, your breasts might be tender, and you can feel some lumps (which appear every month).
The three most common methods of examining your breasts are shown in the figure below. Follow the pattern with smooth touch, and remember to explore the whole breast (e.g, begin at the nipple, later move on to the outer parts of the breast).

Don't panic if you feel a lump in your breast - most of them are benign (non-cancerous). Make an appointment with a doctor and wait for further evaluation.
Screening and prevention guidelines
Women at high risk can undertake some preventive measures, described in an article by M. Costa and P. Saldanha, titled :
1. Tracking by imaging - screening with mammography or ultrasound. It should be performed more often in women with a higher risk. In some cases, a breast MRI is essential.
2. Changes in lifestyle - just like any other disease, its prevention should be based on physical exercise, changing your diet and maintaining a healthy weight.
3. Chemoprevention - selective estrogen receptor modulators, such as tamoxifen, are recommended for women older than 35 years old. Their use can reduce the risk of developing breast cancer.
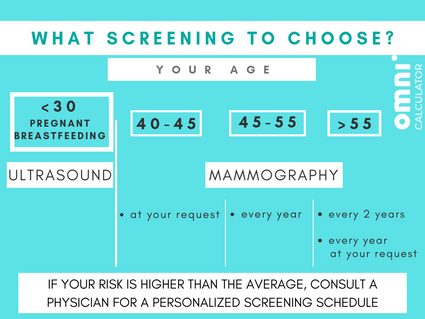
According to the ,
- If a woman is 45, she should begin having her mammogram every year,
- If a woman is 55, she can start having a mammogram every two years. Of course, she can stay with annual mammograms,
- You should have the choice to begin screening at 40 if you want to.
In women who are under 30, pregnant or breastfeeding, an ultrasound is often performed, as mammograms expose the individual to small doses of X-radiation. Check how much with the medical radiation calculator.
If further evaluation is needed, a woman might be referred for imaging with MRI (magnetic resonance), MBI (molecular breast imaging), and a biopsy.
The guidelines above are applicable to women at an average risk. Therefore, if your risk is higher than average, you should consult a doctor and discuss a more individualized and invasive screening.
This tool is not intended to be a substitute for a consultation with your help provider and a professional assessment. It gives approximate results based on risk factors deduced from scientific research. It should be interpreted as a guideline only, and should serve to increase your alertness of the issue. Any worrisome condition should be discussed with your healthcare provider.